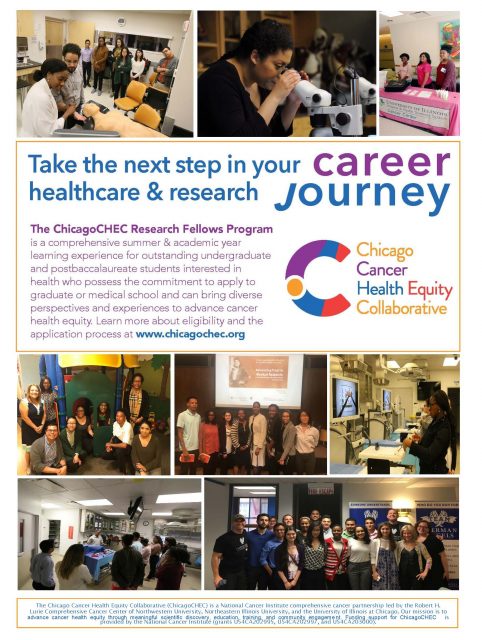
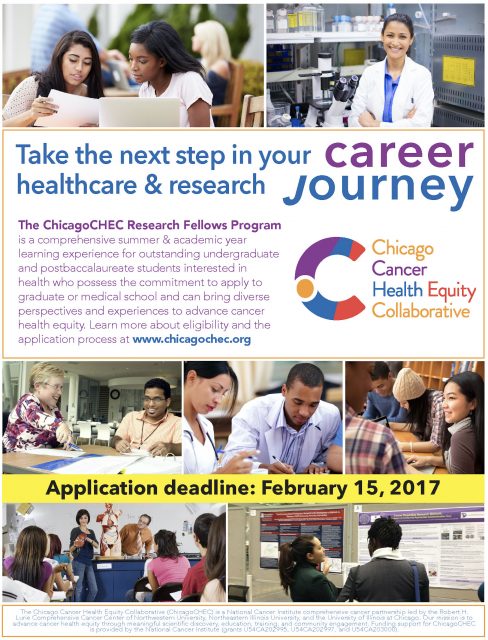
Grounding Experience as a ChicagoCHEC Fellow
Grounding Experience as a ChicagoCHEC Fellow
By: Robynne Alegado
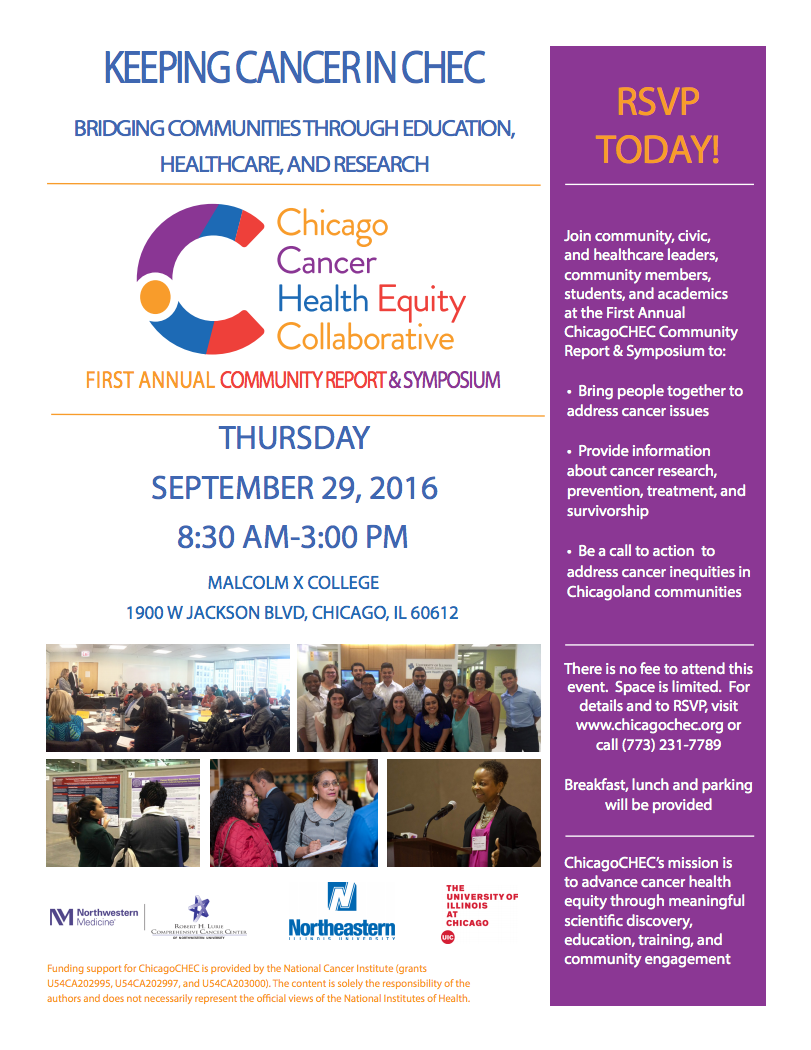
Throughout my journey as a fellow in the ChicagoCHEC fellowship program, I found myself reflecting a lot on continuous cycle of constructing and deconstructing my career plan, finding ways to eliminate healthcare disparities, and learning to be an effective mentor. It was a highly informative roller coaster that put me face to face with the people involved with the healthcare system. I’ve never felt so blessed to be present at every discussion with these inspiring healthcare professionals. I learned a lot about myself, my interests on what I want to pursue, but also how we currently address healthcare disparities. I had an idea of what healthcare disparities were and how much they affected the people around me. It was a battle that seemed simple to beat that required replacing conservative politicians trying to segregate us and being part of the problem not solution. Later on, I learned that it is much more complex to fix the flaws of our healthcare system, and that some aspects may not be fixed in one lifetime. Striving for progress takes time, just like any wound. The wound in this metaphor is inequity. I approached this program with an open mind and attentive ears to see where the problems and solutions related to inequity lie while also structuring my future plans to have a better understanding of myself and the world around me.
My first week as a ChicagoCHEC fellow was quite impactful. My imposter syndrome was kicking in, I felt nervous everyday introducing myself in front of every speaker who wanted a chance to “have a brief idea who their audience was”, and seeing how my role in this group could make a difference in battling healthcare disparities. I continuously thought “why me?” a lot. I had no idea my background and race had something to do with it until we all introduced ourselves and I realized that there were no other Filipinos in the room. I’m not saying being Filipino made me better or worse, it’s just in my experience almost every Filipino I knew went into nursing. I’m also not saying that there’s anything wrong with nursing, but was there something wrong with me picking a career as a physician rather than as a nurse, based on what other Filipinos were doing? This made me wonder if I was wrong in my elevator speech to say that I wanted to be a general physician who does cancer research and that I wanted to go to the Philippines to fight for better healthcare for the poor when I felt so detached from my culture. Why did I feel so alone and different from everyone else? Everyone talked of so much passion and assurance for what they wanted to be. I felt lost, and it made me think that if I can’t help myself, then how do I get millions of people from Chicago and the Philippines to depend on me to provide better healthcare? I was also striving to find a mentor to help convince me that I wasn’t striving for something impossible. It was also during this time that my program arranged Dr. Yancy to speak to us. He said that resilience and continuing to pursue what we want in life while facing any obstacles will be very rewarding at the end when we have reached our goals. This made me aware that my self-doubt and disparities on two parts of the globe were my obstacles and that my resiliency was needed to push myself toward my goals.
I decided to take advantage of my time figuring out specifically what I wanted to do and take action instead of feeling sorry for myself. There was no better time than now to think of the various careers and fields of study that are all part of the healthcare system. I needed to stop thinking of the limits that my racial category and box of a culture that life put me in. I acknowledged it, but I wasn’t going to let it place me in a career I wasn’t satisfied with. I needed to stop the cycle in myself that hindered my self-realization. This coincided with the healthcare system in a sense. It was a continuous cycle that is so deeply rooted into our American society that it is so hard to change. Changing the mind of an individual to change the course of the outcome was simple, but changing the minds of millions of people to take action and change the outcome was so difficult.
When we met fifty high schoolers in one room, all eyes were on us to learn from and meet expectations that probably went through the roof. I had no experience with this generation of high schoolers. They grew up in the modern technological age, which was a few years after me but I couldn’t read them mentally or socially. It got to the point where I gave up over-thinking it and just spoke to them normally like I would my peers. This made me realize our same human approach to patients we don’t fully understand. We just categorize them in one group instead of individually to give healthcare at a faster and convenient rate.
In the later weeks we had some very important speakers that made me want to practice being humble more seriously as well as how I present myself. The oncologist speaker we had as well as Jen Cooper had very informative talks focusing on cancer research and the importance of networking. The importance of these presentations made me think about pursuing an MD/PhD and to basically cast a wide net to find a mentor. Learning about Dr. Moreira’s background highly resonated with my own. It was reassuring knowing that another person who has faced disparities in our medical system, limitations in family and culture, and self-doubt was able to push themselves beyond expectations and find their niche in the medical field. This was heartening to hear to make me put a little more faith in myself and what the future holds for me. His talk motivated me to learn about CAR T-cell therapy and in doing that I was able to make a decision to continue doing research either on the side while being an MD or just pursing an MD/PhD overall. At this point I felt like anything was possible. However, I was taught that without having a strategy on how to show my interest, introducing myself with an elevator speech and posture, it would be close to impossible to find a mentor willing to put time and effort advising me on my career path.
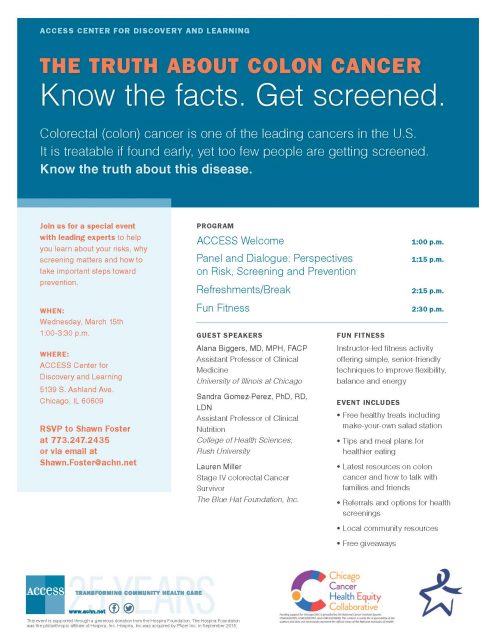
Halfway through the program things started getting more intense. I started learning more about types of cancer therapies available based on how much people can afford, a day in the life of a medical student, and a cancer survivor’s/professor’s talk that just so happened to be positioned at my own university, NEIU. I’ve never met Ben Levi until that day and he was so passionate in his talk that I couldn’t help but be fully engaged. He made me aware of more flaws in the healthcare system where our patients didn’t know the right questions to ask. That we as the healthcare providers should get off our high horse, stop spouting complex medical terminology to scared and confused patients and focus more on translating our information in a form they will understand. This talk emphasized so much on patient care and treatment, especially in the eyes of someone who has literally gone through it and continues to speak his experience. It made me realize that this practice of translational research still needs more improvement and that we as medical providers need to be active towards the change in helping the patient understand more about their disease/illness. The more patient, humble, empathetic, and honest we were towards a patient the more trust they will have in us.
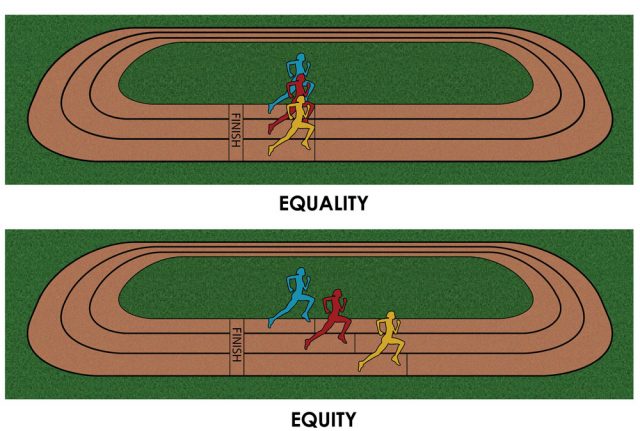
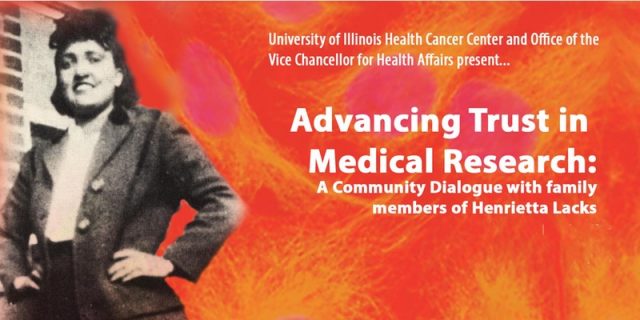
Trust is the number one thing that has been emphasized during the program. It had been abused in earlier years but it can be reestablished with changes in how we approach and address patients. This experience has made me want to learn more about the African American culture, Hispanic culture, and even my own to help establish that trust into different groups to people. I now have a goal to understand, but not assume. I want to learn to communicate on an individual level, to give better patient care and to teach others the importance of this or else the gap in healthcare disparities will continue to expand. I don’t only want myself but for other healthcare providers to be that hope for their patients. The reassurance patients need that they are putting their health into the hands of someone that understands and actually cares about them as individuals. My experience here has motivated me to embrace being different, because being different doesn’t always mean that I am lost. I want to help break that cycle of unequal healthcare and be part of the change that practices patient equity every day.
ABOUT THE AUTHOR
Robynne is a senior at Northeastern Illinois University and is currently interested in pursuing medical school, conducting cancer research, as well as studying healthcare disparities.
Disclaimer
The views expressed in this paper are exclusively those of the author and not necessarily representative of the organizations the author represents nor the ChicagoCHEC organization. This work is solely intended to help further disseminate information related to ChicagoCHEC’s cause and stimulate dialogue about important topics. It is not a report by ChicagoCHEC itself and must not be treated as such.


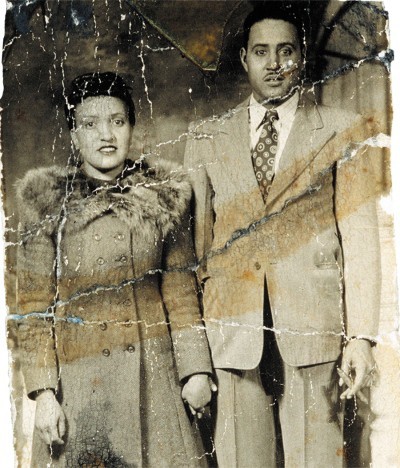 Why is a Culturally Diverse Population of Doctors Needed Anyways? Let’s Take a Walk Down History Lane to Find Out…
Why is a Culturally Diverse Population of Doctors Needed Anyways? Let’s Take a Walk Down History Lane to Find Out…